As people in the UK live longer, demand for residential care and nursing homes is growing ÔÇô as are our expectations of the standard of living they will provide. Max Wilkes of Davis Langdon looks at how home developers and operators are rising to the challenge
01 Introduction
The residential care and nursing homes sector continues to evolve. Government policy has been to encourage elderly people to live independently for as long as possible, which had led to the emergence of the ÔÇťextra-careÔÇŁ sector. This provides specially designed, owner-occupied, self-contained housing, often with round-the-clock support and meals and sometimes with nursing assistance.
Paradoxically, as the elderly population in the UK has grown, the provision of residential care by the NHS and local authorities has shrunk. Improved regulatory standards resulted in the closure of many homes that no longer met the regulations. Today, specialist healthcare companies and registered social landlords (RSLs) are the main providers of new capacity. Their entry into the sector has been funded by institutions looking to diversify their property portfolios, and has resulted in a move to larger schemes with more than 40 beds.
The Joseph Rowntree Foundation has estimated that the number of places required in residential care will increase from about 450,000 in 2004 to more than 1,100,000 by 2050. As people live to greater ages, homes are likely to be required to care for a growing proportion of frail residents, some of whom may have more complicated care requirements related to chronic conditions such as dementia.
A nursing home provides a level of care based on the specific skills of qualified nurses, together with patient supervision up to the level of round-the-clock nursing care. A residential home provides personal care but not at the standard of a nursing home.
Successive reforms of the funding of social care, wider reliance on means-tested benefits and the relative wealth of many pensioners has resulted in a growing proportion of residents of nursing and residential homes being made responsible for the funding of their own care.
A larger group of clients with a financial stake in their care has resulted in residents and their families expecting much better care and conditions than might previously have been deemed acceptable. Combined with the reformed regulatory framework, there is positive pressure to improve the quality and diversity of care home accommodation.
Local authorities and NHS trusts retain a significant role, however, with up to 75% of places in nursing homes being funded by the public sector.
02 Care Standards Act
The Care Standards Act 2000 introduced a wide-ranging regulatory framework for all aspects of social care in the UK. Although it is concerned primarily with the quality of care provided, and the conduct and management of care providers, some aspects of the physical care environment also fall under the act.
The main impact has been the stipulation of minimum space requirements, together with increases in the ratio of en-suite single bedrooms, enabling residents to retain a degree of independence and self-esteem. The act requires that a minimum of 80% of rooms provided are single bedrooms, reflecting the mostly single demographic of residents.
These factors have resulted in more than 95% of new-build care homes under construction being designed for single-bedroom occupancy.
For existing businesses, the costs of meeting these requirements, coupled with diminishing returns from fees for placed residents, has resulted in the closure of many homes over the past few years.
03 Funding and procurement
Under national planning guidance and councilsÔÇÖ local plans, purpose-built housing for elderly people is best located close to transport links, and facilities such as post offices, shops, chemists and doctors. Based on these needs, many developments take place on brownfield sites in existing residential areas.
For larger nursing homes run by private-sector operators, there are two main routes for the long-term funding of developments:
ÔÇó PropCo/OpCo The business is spilt into two arms: the property holding company (PropCo), which leases the development to an operating arm (OpCo). The advantage of this approach is that it offers the potential for the business to increase the leverage of its capital, as borrowing can be secured against the property asset via the PropCo and against business revenues via the OpCo. These arrangements are inevitably complex and a drawback is the potential for conflicts of interest between the PropCo and the OpCo.
ÔÇó Sale and leaseback This approach is favoured by larger operators that sell completed projects to a financial institution and lease them back. This arrangement allows operators to concentrate on their core businesses and to release capital value in order to fund future developers.
The introduction of real estate investment trusts (REITs) into the UK market could also prove an effective vehicle for investment in this sector, particularly for smaller investors that need some degree of securitisation. The main focus for REITs is properties that offer rental incomes.
Opportunities for pension-related investments via self-invested personal pensions or small self-administered schemes are also bringing further investors into the sector.
Procurement
The two main client groups for nursing and residential care homes ÔÇô registered social landlords and private healthcare operators ÔÇô are experienced businesses that understand their requirements and are knowledgeable about the construction market. Given the size and relative simplicity of these buildings, the main procurement routes used are either a traditional lump-sum or design-and-build contract.
In the past, a common criticism of the care and nursing home sector was that the quality of the care environment was often compromised by the physical limitations of existing buildings and by tight budgets. This is much less true today, with providers generally being motivated to provide generous space standards, good-quality finishes, effective use of natural light and control of noise.
While standards are generally well understood, the project team still requires a clear brief with regard to the planned caring regime, especially if it is anticipated that some of the residents may suffer from chronic conditions such as dementia. Smaller-scale operators with less experience will rely on the knowledge of the project team to deliver an appropriate solution.
04 Design considerations
Guidelines for accommodation areas are laid out in the 2004 revisions of the Care Standards Act 2000. The following considerations should be taken into account.
- Small scale units of between 8 and 15 bedrooms are considered to be the best-sized for providing a homely, less institutional environment.
- Cost-effective use of space is important, in particular related to the provision of ancillary spaces. An allowance equivalent to 25% of net space is required for circulation.
- The layout of care homes should be as simple as possible, offering good sight lines to enable staff to monitor the residents.
- All en-suite bathrooms should be designed to enable a wheelchair turning circle. Many elderly people find showers easier to access and use than baths. An assisted bathroom should be provided per eight residents.
- Multiple communal areas should be provided for residents to socialise, undertake organised activities and to meet relatives.
- Small kitchens may be located next to each ÔÇťclusterÔÇŁ of bedrooms, together with lounge, dining area and toilets.
- Where practical, garden landscaping visible from bedroom and dayroom windows should be provided.
- Wheelchair and ambulant access to the building and gardens must be considered with pathways wide enough for two people and the use of ramps in place of steps.
- The police initiative Secured by Design is the generally accepted personal security standard for registered social landlords.
- Recent amendments to Part B on fire safety mean that where there is only one bed per room, free-swing closing doors may be used. Where there is more than one bed in a room, sprinklers must be specified.
- Central heating should be provided to all rooms, with controls in individual bedrooms. To prevent injury, all pipework and radiators must be guarded or have low-temperature surfaces.
- Background lighting levels of 150 lux are appropriate in residentsÔÇÖ accommodation, supplemented by provision for table level lighting.
- Natural light should be maximised in communal areas. Artificial lighting should be carefully specified so as to avoid creating an institutional atmosphere.
- Hot water storage is governed by measures to prevent legionella, being stored at 60┬░C and circulated at 50┬░C. Good practice dictates that water is locally distributed at 43┬░C.
- Provision for high levels of general hygiene is important in order to support the health and well-being of residents. Laundry services are typically provided on site, while a sluice room should be allowed for each bedroom cluster, located away from WCs.
06 Cost model
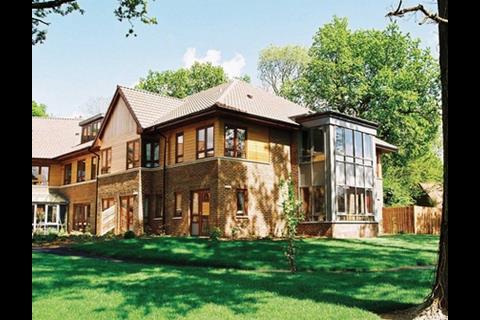
The cost model is based on a two-storey extension to an existing nursing home. It has 16 single bedrooms, each with an en-suite bathroom. Each floor features a kitchenette, dayroom, ancillary space and an assisted bathroom, giving a gross internal floor area of 650m2.
The building is constructed using a traditional facing-brick cavity wall on strip footings with precast concrete floors. The roof is constructed of concrete tiles on softwood trusses, the windows are PVCu and the internal partition walls are blockwork.
Services include gas-fired heating systems with low-surface-temperature radiators, lighting and nurse call alarms.
The unit rates are derived from design-and-build tenders and are current at the second quarter of 2007, based on a West Midlands location.
The building-only cost is ┬ú1,200/m2, which equates to ┬ú48,750 per room. This compares to mid-quartile costs collected by the ║┌Â┤╔šă° Cost Information Service of ┬ú950-1,350/m2 for nursing homes and ┬ú1,050-1450/m2 for old peopleÔÇÖs homes.
The costs exclude enabling works, external works and external services. The costs of non-fixed furniture and fittings are omitted, as are professional fees and VAT. Unit rates should be adjusted for location, site conditions, programme and procurement route.
Downloads
Cost breakdown: nursing home extension
Other, Size 0 kb

























4 Readers' comments